Eating disorder not otherwise specified (EDNOS), the catch-all diagnosis for eating disorder patients that don’t neatly fit into the DSM-IV anorexia nervosa (AN) or bulimia nervosa (BN) categories, is often thought to be less severe. Patients with sub-threshold AN or BN (missing one or two criteria) fall into the EDNOS (a large proportion, perhaps the majority, of patients). The inherent assumption in the word sub-threshold is that the patient is not as sick. Symptom frequency and behaviours are not that bad.
Increasingly, research is showing otherwise (which comes as no surprise for those of us who have struggled with eating disorders).
One study that has illustrated this quite nicely was published in 2009 by Dr. Scott Crow and colleagues in the American Journal of Psychiatry. Given that most ED mortality research has focused on anorexia nervosa, Crow et al wanted to compare mortality (from all-causes and suicide specifically) in patients with anorexia nervosa as well as bulimia nervosa and EDNOS. Furthermore, they were interested in studying a heterogenous sample over an extended period, as opposed to fairly homogenous, short follow-up studies.
Patient Demographic and Characteristics
- 1,885 outpatient (treatment-seeking) individuals that were evaluated at the Outpatient ED Clinic at the University of Minnesota between 1979 and 1997
- 1/20 were male
- AN: 177 patients, BN: 906 patients and EDNOS: 802 patients (diagnosis made at the time of evaluation at the Clinic, not lifetime diagnosis)
- The median age was mid 20’s for all groups (slightly younger for AN, unsurprising given the diagnostic crossover data in literature).
- over 90% were white (it is Minnesota)
- the follow-up was slightly over 18 years (on average)
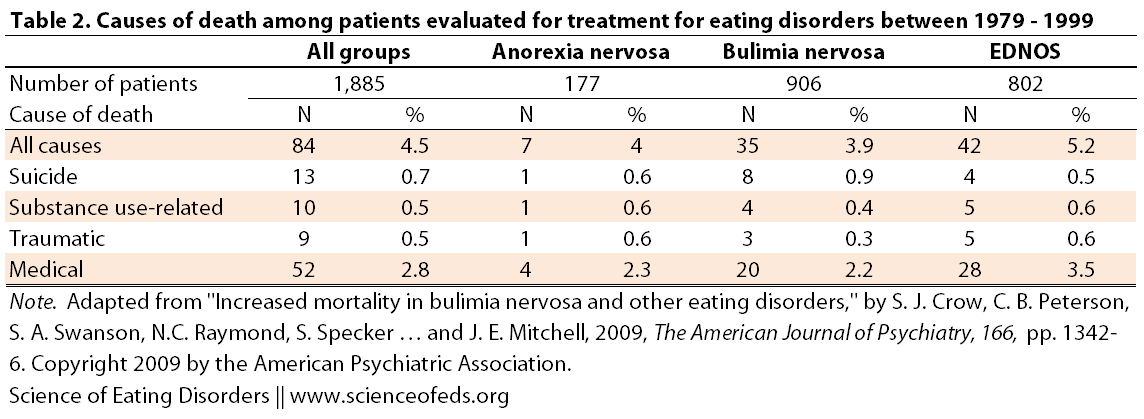
Crow et al relied on the National Death Index database compiled by the National Center for Health Statistics for their data and classified the causes of death into suicide, substance use-related, traumatic and medical.
Some definitions:
Crude mortality/death rate: mortality rate from all causes of death for a population in a given time period (usually the total number of deaths per 1000 people/year).
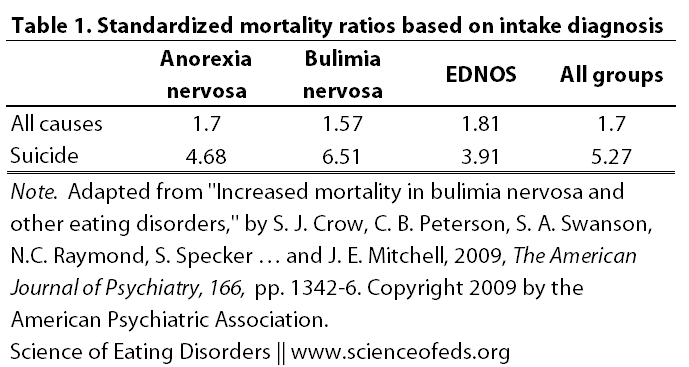
SMR = standard mortality ratio: is a ratio between the observed number of deaths in the study group and the number of deaths that would be expected (based on demographic characteristics [age, sex, race, calendar year specific national mortality rates]). If the ratio of observed:expected deaths is greater than 1.0, there are more deaths in the study population than would be expected in the general population. Wikipedia gives a nice example:
“An SMR for bladder cancer of 1.70 in the exposed group would mean that there is 70% more cases of death due to bladder cancer in the cohort than in the reference population (in this case the national population, which is generally considered not to exhibit cumulative exposure to high arsenic levels).”
Here’s the breakdown of the SMRs based on different diagnoses (at admission):
First, the SMR and mortality rate for AN are lower than reported in many studies, this could be due to several factors:
- this study evaluated outpatients, not, as in most earlier studies, inpatients (which can be interpreted as being less severely ill)
- ~ 18 year follow-up is longer than many other studies, which increases the expected deaths in the population (denominator), thus, decreasing the overall ratio of observed:expected deaths,
- classification was based on current versus lifetime (original/initial) diagnosis [which is why there were less patients in this category], limiting the statistical power, but also
- in previous studies, using lifetime diagnosis would have resulted in patients who, at the time of death had BN or EDNOS, were actually classified into the AN category
This would suggest that this SMR value is actually more realistic and reflective of the AN population (although, it is unclear if it is reflective of the non-treatment-seeking sample, that’s naturally very hard to evaluate).
BN and EDNOS rates, however, are higher than in many other previous studies. Perhaps this is because the sample of BN and EDNOS patients is quite large (906 and 802, respectively), and perhaps therefore, more reflective on these populations.
As the authors note, it is quite possible that the elevated mortality and SMRs in EDNOS is actually contained in a small subset of the group, given than EDNOS was, literally, everyone with an eating disorder that didn’t fit AN or BN (in other words, a very heterogeneous group). This is something that will be very important to evaluate in future studies, especially to strengthen the empirical validity of the upcoming DSM-V diagnostic criteria.
Table 2 further subdivides the deaths by the cause (suicide, substance use-related, traumatic or medical). While this is interesting, the absence of SMRs makes it difficult to evaluate with respect to the non-ED population at large. It is also not defined exactly what traumatic and medical mean, which would have been nice – just to know your guess based on the name is correct.
In the future, it will be important to also monitor and keep track of the changes in a patient’s diagnosis (perhaps not quite as frequently, but similarly to Eddy et al., 2008 and 2010), particularly at the time of death, to account for diagnostic crossover. It will be important to combine datasets from many areas around the country (and in other countries), particularly to evaluate any differences in mortality between different racial groups (ie, to conduct a multi-site study).
An important note on exclusion: obese patients with binge eating disorder were not included in the EDNOS category (because they were referred to a different, obesity-focused clinic).
The authors also state something that I haven’t previously thought of, but now appears obvious: the underreporting of suicide as a cause of death, which makes determining the real number of suicides in the ED and non-ED populations, and how they compare, rather challenging. I guess the assumption is that this bias in underreporting is similar for both the observed and expected groups?
The take home message here, as I see it, is:
The common perception of eating disorder not otherwise specified as a “less severe” eating disorder thus seems unwarranted.
And, context matters: note how different these findings are from the meta-analysis I blogged about in my previous post. Characteristics and demographic of the sample population, as well as the methodology, greatly influence the results in these studies, and it is crucial to carefully assess this, in evaluating the evidence and it is generalizability.
References
Crow, S.J., Peterson, C.B., Swanson, S.A., Raymond, N.C., Specker, S., Eckert, E.D., & Mitchell, J.E. (2009). Increased mortality in bulimia nervosa and other eating disorders. The American Journal of Psychiatry, 166 (12), 1342-6 PMID: 19833789