A not-so-recent, but interesting paper by Cynthia Bulik and colleagues outlines an interesting model for perinatal risk factors in the development of anorexia nervosa. The model “focuses on adverse perinatal events and prematurity as risk factors for AN and encompasses the potential role of passive gene-environment correlation in perpetuating AN risk.”
Importantly, this model “provides intriguing data on a potential cycle of risk for at least a subset of individuals with AN.” The word subset is important: this model, if true – and we don’t know yet, undoubtedly applies only to a proportion of individuals that develop anorexia nervosa, so keep that in mind.
(In case you are wondering, because I was, perinatal period starts at 140 days of gestation and ends 28 days post birth, prenatal period is any time before birth.)
Trying to figure out the risk factors for anorexia, a rare disorder (<1% of the population), is challenging. One of the best ways to determine real risk factors (as opposed to early symptoms, such as dieting and overexercise) is to do longitudinal prospective studies: tracking lots of people over an extended period of time, and then seeing who develops AN and who doesn’t. Then you go back over all of that data you collected and try to determine common factors share by individuals that developed AN. But, if for every 100-150 people, 1 person develops AN, it is easy to see that you have to track a lot of people to identify true risk factors. And then, of course, anorexia itself is not a homogenous disorder.
PERINATAL RISK FACTORS FOR AN
- premature birth, particularly if small for gestational age (SGA) (Cnattingius et al., 1999)
- born with cephalohematoma (blood hemorrhage between the skull and one of the layers between the skull and the brain called the periosteum) (Cnattingius et al., 1999)
- another study, looking at the same data, determined “that perinatal risk factors attribute a 3.6% risk for cases of AN” – not large, but statistically significant (Lindberg et al., 2003 )
Cnattingius et al. hypothesize that mild brain damage could lead to difficulties in eating during infancy, and that might be a contributing factors toward AN. I’m not sure I’m sold on that explanation, but whatever the answer, the data itself is quite intriguing.
Bulik and colleagues propose an alternate explanation that seems more plausible to me. Children of AN women have an increased risk of developing eating disorder – that’s been known for some time. But, anorexic women, even after recovery, are more prone to maintain a low body weight and “experience higher than expected rates of pregnancy complications.”
In other words, could premature birth and SGA be, at least in part, the result of undernutrition due to anorexia (or anorexic symptoms, even in those that could be classified as recovered)?
Interestingly, Bulik et al. mention a study that found “no difference between women with a history of AN and controls on the rate of pregnancy, mean number of pregnancies/woman, or age of first pregnancy.” That’s kind of contrary to what I assumed, to be honest.
But, expecting mothers with AN, or history of AN, do need to be careful and be aware of the risks and complications that care arise:
- “higher rate of miscarriages”
- “higher likelihood of cesarean deliveries”
- “low prepregnancy weight and low weight gain during pregnancy are associated with low infant birth weight… higher incidence of congenital malformations”
- birth complications include: “stillbirth, low birth weight infants, low Apgar scores, higher occurrence of breech presentation, and cleft lip and palate.’
- “higher rates of perinatal or infant loss in mothers of a clinical sample of individuals with AN and greater maternal anxiety, concern during pregnancy.” (Shoebrige and Gowers, 2000)
On the positive and preventative side, one study found that “when women with AN gained adequate weight throughout their pregnancies, the complication rate did not exceed population expectations nor did the rate of observed birth defects.” (Namir et al., 1986)
Furthermore, undernutrition in women was found to increase corticotrophin releasing hormone (CRH). CRH triggers the release of stress hormones.
Bulik and colleagues hypothesize:
Women with prolonged periods of no food (including beverages) were more likely to have higher CRH concentrations levels during pregnancy and deliver at a shorter gestational age. Thus, it is possible that prematurity and SGA were secondary effects of lingering suboptimal nutrition possibly secondary to lingering eating disorders symptoms in the mothers during pregnancy.
GENE-ENVIRONMENT INTERACTIONS
I’ve written before that anorexia, and eating disorders more broadly, run in families. This is due to both genetic factors (as illustrated by high heritability values), but also shared environmental factors. What’s more, parents can pass on genes that predispose someone to developing AN, but then raise them in an environment whereby those genes are, in simple terms, turned on. Bulik calls it a “double disadvantage”: “Not only are they likely to inherit genes that influence risk for AN, but they may also be exposed to environments that are in part shaped by the parental genotype that increase the likelihood of expression of the underlying risk genotype”
Mothers, of course, are well-meaning and don’t expose their children to such an environment on purpose. But, anorexic thoughts and behaviours, even after recovery, can be very difficult to extinguish. Things like the amount of months spent breastfeeding, anxious and tense attitudes during meals, and of course, a focus on appearance.
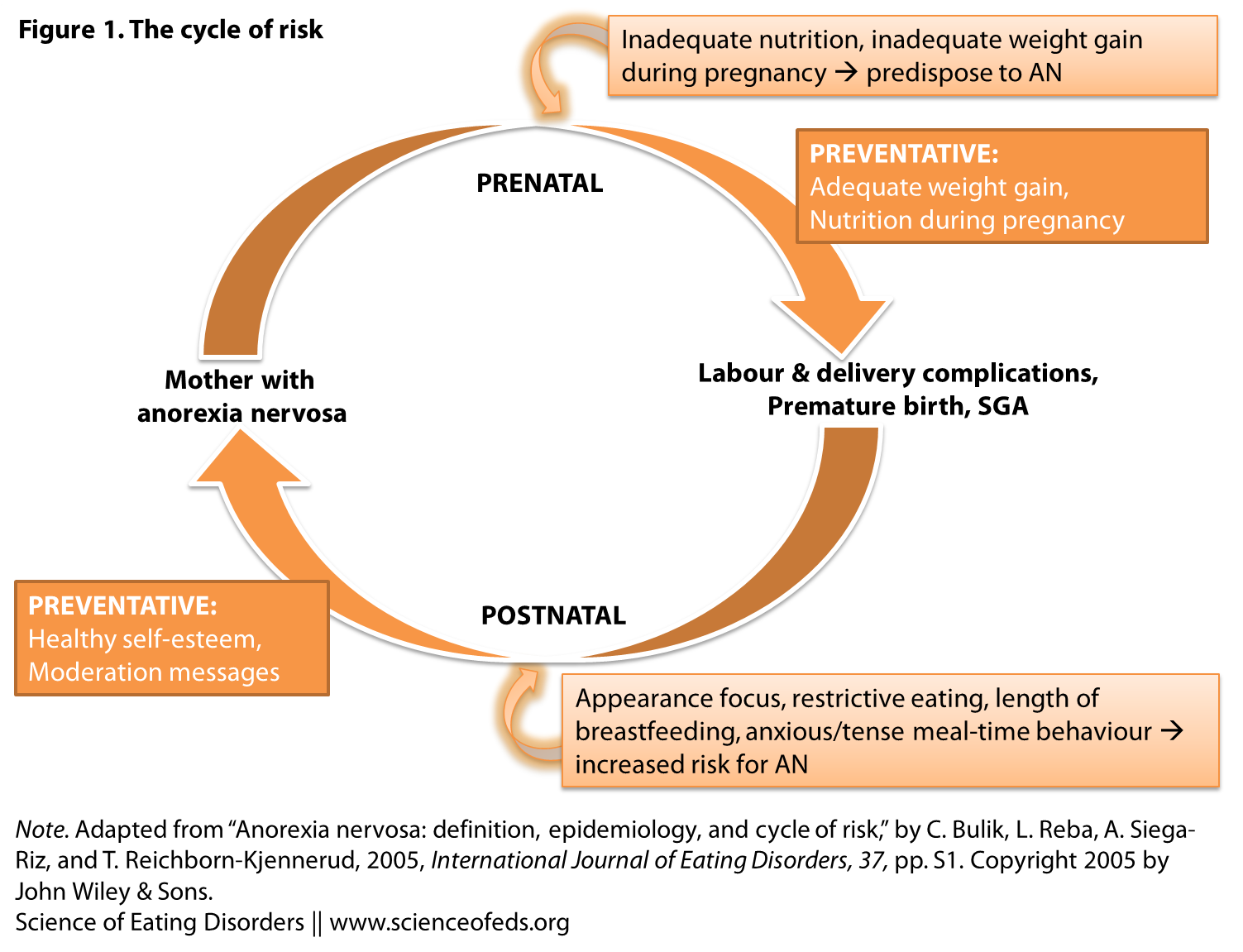
Combining all of the information above, Bulik and colleagues put forth this “Cycle of Risk” model (I modified it slightly and made two figures into one):
It is self-explanatory, but here’s a short explanation nonetheless: Mothers with AN are less likely to gain enough weight and eat enough during pregnancy, leading to premature birth and SGA, which have been shown to be risk factors for AN (Cnattingius et al., 1999). Moreover, during early childhood development, they are exposed to environmental factors stemming from a history of AN, sub-threshold or full-syndrome AN in the mother (unlikely to be intentional, of course). This further exacerbates the risk for AN, and the cycle continues.
Again – it is important to stress that if this model is true, it is certainly not the cause of anorexia nervosa for everybody. Clearly. It is a possible risk factor and cause for a proportion of those individuals that go on to develop anorexia.
In any case, this is pretty interesting stuff. And in the last 7 years since this paper, Bulik and team have published several research studies that seem to support this model. I’m planning on writing about some other studies on this topic in the near future.
FOR MORE ON THIS TOPIC, check out Dr. Cynthia Bulik’s lecture here. My favourite part is from around 8:40-10:00.
References
Bulik, C., Reba, L., Siega-Riz, A., & Reichborn-Kjennerud, T. (2005). Anorexia nervosa: Definition, Epidemiology, and Cycle of Risk International Journal of Eating Disorders, 37 (S1) DOI: 10.1002/eat.20107
Another interesting fact from our Norwegian study is that over 50% of pregnancies in women with anorexia were unplanned, compared with 19% in women without eating disorders. We wondered whether this is because women *mistakenly* thought that since they weren’t menstruating, they weren’t fertile. This is not true. You can still be ovulating even though you are not menstruating regularly or at all. This also means that if you are irregular, you might miss out on the major signal that you are pregnant–namely missing a period. Which means it might be later into your pregnancy that you start doing health-promoting behaviors like eating healthfully and taking supplements. It does seem in our study too, that adequate nutrition and weight gain during pregnancy for women with anorexia nervosa may contribute to healthy pregnancy outcomes.
Thank you so much for your comment Dr. Bulik! That’s really important to know, particularly to recognize pregnancy early and get adequate nutrition and weight gain. I’m glad those those interventions help.
You can still be ovulating if the hormones aren’t completely pancaked – it might not be sufficient to menstruate but enough to get pregnant? Is that correct?
Hi. this is very interesting. Can you tell us more about how the length of time of breastfeeding may or may not affect risk factors?
Hi Deborah, thanks for commenting!
From the top of my head, I don’t know. I do believe Dr. Bulik mentioned it in the lecture (link above, at the end of the post.)
This is freely available on-line and it may interest you:
“Reproductive Issues in Anorexia Nervosa”
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3192363/?tool=pubmed
I’m not sure to what it extent it is known HOW the length of time affects risk factors – I simply haven’t done enough research into this area, unfortunately.