I don’t know how many times I’ve said, “I’ve already eaten, thanks,” “No thanks, I’m going be eating later,” or “I’d love to, but I’ve got a stomach ache,” when I actually hadn’t eaten, wasn’t going to eat later, and didn’t have a stomach ache. Why did I do that? Did I realize I had, or was developing, an eating disorder? How long did it take for that realization to click? And once it did, did I stop lying to avoid eating with others or did I do it more?
A lot of questions spring up when you start thinking about secrecy, denial, and lying as it related to eating disorders. And answering these questions by having to remember what you thought when you first began to show signs of your eating disorder is hard. It is hard for many reasons, but one reason is that the we feel about events in the past is inevitably coloured by our experiences since then. That’s important to consider when thinking about the data in the study I’m about to discuss.
A little diversion: there are a lot of things that can bias research findings, and while it is important to try to minimize them, I feel it is much more important to be aware of them, so that data can be interpreted accordingly. It is impossible to rid research of all biases (I think, anyway) but it is crucial to be aware of the ones that may significantly impact any particular study. Just check out how many various memory and cognitive biases there are: memory-biases and cognitive-biases. Lots!
But anyway, let’s get back to the present study. In this paper, Dr. Walter Vandereycken and Dr. Ina Van Humbeeck, utilized a retrospective survey approach to get an idea of how patients dealt with the realization and recognition of their emerging eating disorder.
In other words, they wanted to understand “the extent and meaning of denial at the moment the subjects are denying either due to distorted information processing or to refusal of self-disclosure.”
First, they classified denial into two major categories:
- unintentional denial, a sort of impaired self-awareness, if you will
- intentional denial, a deliberate refusal to disclose information, “faking it,” if you will
But in order to get at the idea of how patients felt and what behaviours they engaged in when their eating disorders were just emerging, Vandereycken and Van Humbeeck had to rely on answers from patients who were passed the stage of unintentional denial (if they ever experienced it in the first place). They chose to use a survey. I would’ve done interviews, because as you’ll soon see, a lot of participants put “not applicable,” meaning that the survey wasn’t able to capture a lot of the variation in people’s behaviours and thoughts. The benefit however is that they were able to survey 401 individuals, a sample size that’s probably impossible to get for an in-depth interview study. Interestingly, the authors’ rationale for using a survey was to conduct a more systematic assessment of the experiences, but as I’ve stated, I feel like they are missing a lot of the richness that they would’ve gotten if they had done interviews.
On average, the participants were 25 years old (range: 15-54), and there was an fairly equal split between anorexia nervosa restrictive subtype (~25%), anorexia nervosa binge-purge subtype (~25%), bulimia nervosa (~30%) and EDNOS (~16%).
Importantly, the eating disorder diagnoses were based on self-reported data, so there’s no way of knowing whether the data would be the same if individuals were evaluated by clinicians. Moreover, we have no way of knowing if these are their present diagnosis, their initial diagnosis, or the diagnosis that the associate with the most (perhaps they experienced a lot of diagnostic crossover, but spent more time on one side of the spectrum).
The average time between the onset of the ED and the present age was 9 years, and most of the participants categorized themselves as either considerably improved (20%) or moderately improved (42%).
Hilariously, they forgot to ask about gender. I’m not kidding. They assumed it was roughly 95% female based on the membership of the organizations from where they recruited their subjects. (I’m not going to lie, I laughed out loud, literally, when I read that in their “Methods” section. How can you forget such a basic thing? It is silly.)
They asked the participants to “return in imagination to the beginning stage of their eating disorder: ‘Patients who currently are in that phase cannot reliably reflect upon it, for they are inclined to use a distorted—better or worse—view than in reality. You are further on and may look back in a more honest way, even if you feel sad, angry or ashamed about that period in your life.’”
The questions were divided into two main categories:
- “behaviours used to hide the eating disorder and cope with reactions from the social surroundings”
- “cognitions about the eating disorder at that time (knowledge, impact, significance)”
Here are the results.
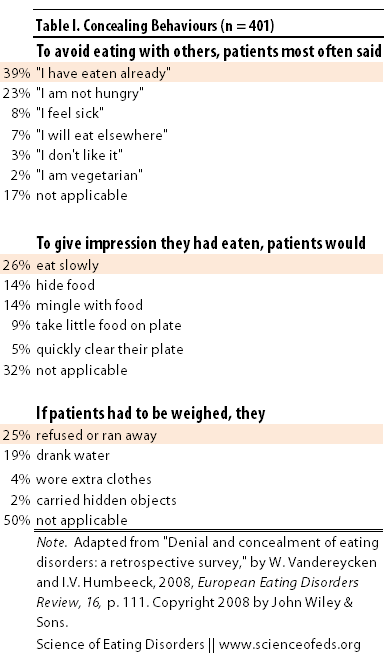
The first table summarized the data about behaviours used to hide eating disorder behaviours. As you can see, for a substantial amount of people (from 17%-50%), none of the options were applicable. I would’ve loved to see what these participants had to say. Did they not engage in any of the behaviours or where the concealing behaviours they engaged in not listed from the few options? I’m sure you’d agree that is an important distinction.
Moreover, participants could only pick one option. I would’ve preferred if participants were able to select all that applied.
The authors also asked the participants how consciously they acted to conceal their eating disorders behaviours: “the majority report the concealment as a deliberate strategy with respect to avoidance of eating together (58%), false impression of eating (57%) and manipulating weight (73%).”
That’s interesting to me. I never did anything to manipulate my weight or give a false impression of eating more than I was, but I did often use those excuses to get out of eating. (And I often got defensive if more food was pushed my way.) In part, it wasn’t concealing my eating disordered behaviour, but knowing that eating outside of my plan/schedule, would make me anxious, and I wanted to avoid that.
The next question the participants were asked was how they reacted when people made remarks about the aforementioned behaviours. As you can see in table II, the most common responses were that the participants felt the people were exaggerating their disordered behaviours (‘it wasn’t that bad’) or falsely accusing them of something they didn’t think was true or didn’t admit to publicly. I can definitely say that I would’ve fallen more into the negative reactions category, but not because I thought they were exaggerating or falsely accusing me, mostly that I just didn’t want to talk about it.
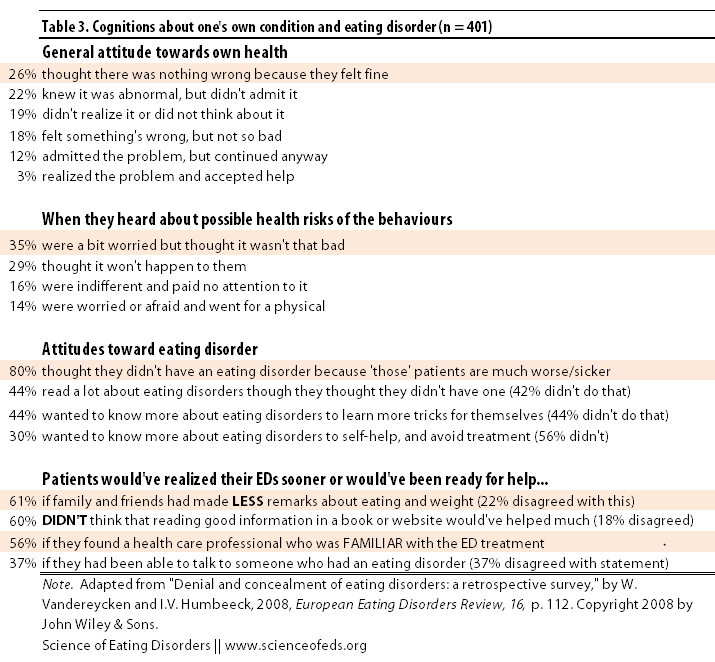
Next, the participants answered questions regarding their own understanding of the disorder during those early stages (Table III). I picked out what I thought were interesting or important parts of the data reported in this paper. As you can see, really early on, a quarter of the participants thought that there was nothing wrong, and about a fifth did realize that something was wrong, but didn’t admit to it.
That’s interesting. I realized that I had a problem really early on. Before I even lost any significant weight. So, I never denied I had a problem. I sought help personally, and frankly, fought for it. I’m not sure why I was so aware of the situation, perhaps because none of my friends ever dieted, not to my knowledge anyway, so my restrictive behaviours were really odd compared to my group of friends? Or maybe it was because we had just covered eating disorder in health class the year before? I’m honestly not sure.
Again I feel that so much information is being left out. For example, I’m sure initially, I felt that nothing was wrong (don’t we all at the VERY start?), or perhaps I didn’t think about, then I’m sure it started to sink in but I didn’t think it was that bad, and perhaps when it finally sunk in (still early on, for me), I knew I had a problem but I couldn’t stop. Unfortunately, I feel that this evolution of how people felt during the early stages, the progression or the order of when different feelings became more prominent, is left out due to how these data were collected.
The most striking thing from Table III, which I think may be counter-intuitive, is that 3 out of 5 participants said that they would’ve realized their EDs sooner, or would’ve been ready for help sooner if their friends and family made FEWER remarks about eating and weight. What’s more, an equal amount thought that information on the web or from books wouldn’t have been very useful, BUT finding a health care professional who was familiar with eating disorders would’ve been (at least for roughly 50% of the participants).
Information about the possible health risks of eating disorders made little impact on the patients. That’s something that’s completely unsurprising to me.
Reading the discussion, which I am not quoting here, I felt that the authors thought that denial or concealment of eating disorder behaviours was somehow mean-spirited, or something.
For me, concealing whether or not I had eaten were just ways to ease my anxiety. Eating already made me anxious, but eating in a foreign place, eating food that I didn’t know the calorie content of, around people that I wasn’t friends with, at a time that wasn’t my usual meal time, was hugely anxiety provoking. I didn’t lie to mislead others as much as I lied so that I wouldn’t have to deal with the guilt I would’ve had to face if I were to eat.
In the discussion, Vandereycken and Van Humbeeck talk a bit about the clinical relevance of these findings.
Why do more than half of our respondents believe they would have recognized their eating disorder earlier if they had met a health care professional who was familiar with this disorder? Why would they be more open to someone who has specialized in the treatment of a disorder they claim they don’t have? We suppose that a well-balanced confrontation within a context of support and understanding is crucial in the process of problem recognition. Though one can speculate about these and other clinical implications, the findings of this survey support our conviction that in many cases ‘denying’ should be translated as ‘not admitting’ (Vandereycken, 2006b).
Overall, the findings are not too surprising for me.
Readers, what do you think? Do you remember what you were like in the early stages of your eating disorder (or parents, what your children were like)? How do you make sense of those behaviours now? What do you think would’ve helped you recognize and seek help earlier than you did (if you sought it out relatively late)? What helped you recognize it eventually?
References
Vandereycken, W., & Van Humbeeck, I. (2008). Denial and concealment of eating disorders: a retrospective survey. European Eating Disorders Review, 16 (2), 109-114 DOI: 10.1002/erv.857