Exercise can be great for your body and for your mental health. It is well accepted that exercise can decrease anxiety, increase concentration, and generally improve mood. But too much exercise can be harmful, especially during recovery from a restrictive eating disorder. So is there a way to reap the benefits of exercise without the risks? And if yes, can this exercise actually help in the recovery process?
One form of exercise that has gained a lot of popularity is yoga. Initial studies on the use of yoga in treatment of anxiety and depression seem promising (though I haven’t checked them out in detail myself) (Mishra et al., 2001; Sahasi et al., 1989; Pilkington et al., 2005; Mitchell et al., 2007). So, can it be used as an adjunct with regular eating disorder treatment? Can it decrease eating disorder symptoms?
In this randomized controlled study (RCT – randomized controlled trial), Tiffany Rain Carei and colleagues wanted to see whether standard care with individualized yoga was more effective than standard care alone in the treatment of eating disorders for individuals between the ages of 10-21.
PARTICIPANTS
Patients were recruited from Seattle Children’s outpatient eating disorder treatment unit and had to meet the DSM-IV criteria for anorexia nervosa, bulimia nervosa, and/or eating disorder not otherwise specified (EDNOS). Exclusion criteria included, among other things, the inability to participate in yoga as determined by the treatment team and co-morbid psychotic, conversion, substance-abuse and/or axis II disorders (developmental disorders and personality disorders).
They enrolled 54 adolescents (50 females, 4 males) and four females dropped out, leaving 50 who completed the study. The average age was 16.5 and the mean length of illness was 14 months. Over-exercising was reported by 48% of the participants (prior to the start of the study). A similar amount were hospitalized prior the study. The breakdown for AN, BN and EDNOS was 55%, 17% and 28%, respectively.
Importantly: some study participants were doing individual psychotherapy (16), art therapy (14), and/or were on SSRIs (12). However, these participants were equally distributed across the two groups.
They randomized the individuals into the (i) yoga and (ii) no yoga groups but made sure that every group had equal number of AN, BN and EDNOS patients (stratification).
YOGA INTERVENTION
The participants in the yoga group received two one-hour yoga sessions for 8 consecutive weeks. Each participant had one-on-one instruction with a Registered Yoga Teacher (RYT). All RYTs were trained by the same instructor in the same studio and sessions were taped to ensure that instructors were following the protocol.
OUTCOMES
All participants were assessed using the Eating Disorder Examination (EDE) prior to the start of the study, immediately after the intervention and one month following the intervention. Depression was measured using the Beck Depression Inventory, anxiety was measured using the State Trait Anxiety Inventory, and food preoccupation was measured using a modification of the EDE.
So… what did they find?
MAIN FINDINGS
Did eating disorder psychopathology improve?
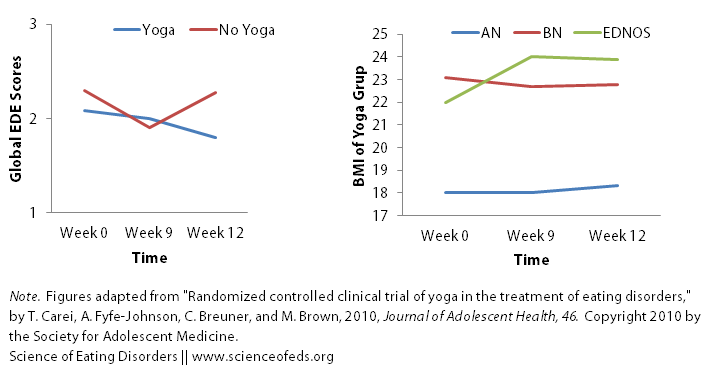
- Kinda-ish-not-really. At the end of the treatment for the yoga group, the yoga and no yoga groups did not differ in the EDE scores, but the group that received yoga treatment experienced a decrease in eating disorder psychopathology following treatment whereas the group that did not experienced an increase. But, overall, the findings were not significant.
- There were no effects if you were to break down the EDE into its components (restraint, shape concern, weight concern, eating concern)
Did general psychopathology (depression, anxiety) improve?
- Both the no yoga and yoga groups experienced a decrease in depression and anxiety but there were no significant differences between the two groups.
What about weight?
- The BMI values in both groups didn’t really improve over the course of the study for the AN group… (they were in the normal range for the BN and EDNOS groups). It improved or stayed the same for 62% of the participants and decreased more than 0.5 points for 18%.
- There were no significant changes in the BMI for the yoga and no yoga groups (if you compare those with AN versus BN versus EDNOS)
- But this means that yoga did not adversely affect BMI.
What does all of this mean?
I think there are two key points in this study: (1) 2 hours of a yoga a week did not negatively affect BMI and (2) participants who did 8 weeks of yoga experienced less eating disorder psychopathology symptoms (as measured by the EDE) 1-month after the intervention.
This study is one of the first (if not the first) RCT on yoga in the treatment of eating disorders. RCTs are considered a gold-standard in this line of research. I’m very happy to see this. Especially after reviewing that particularly awful junk study without a control group (here). Sure, the results aren’t miraculous: but they are real. The numbers are not spectacular, but it is what we would expect in the real world (not a perfectly clean study).
I also think this study provides a good precedent for future studies, since it has nicely shown that some level of yoga doesn’t negative affect treatment (which is what one would be worried about when it comes to exercise during ED recovery).
As I read it, I thought: is 2 hours/week enough? Is 8 weeks enough? I’m not a yoga person (I’ve tried and really didn’t like it) but I do exercise a fair amount. I also love walking. Which makes me think: would two hours a week make a big difference on my mood, anxiety, depression and eating? Probably not. I need way more. (I picked walking because unlike distance-running, it is not very cardio-intensive and maybe quasi-analogous, but like I said: I don’t do yoga.)
After all,
Participants frequently endorsed this qualitatively [reduction in food preoccupation] after yoga sessions, commenting “This is the only hour in my week when I don’t think about my weight.”
Since they’ve shown that yoga is not a negative add-on (and may be positive), it would be great to see a follow-up study that’s involves more yoga, and for longer.
The limitation of the study (meaning that you shouldn’t generalize to other situations) were that the the participants were outpatient adolescents with short ED histories.
We don’t know if the findings hold true for inpatient or community samples. We don’t know what the results would look like for an adult population (better or worse)? Or what about the differences between anorexia nervosa and bulimia nervosa patients (yoga is more effective for a particular subgroup of ED patients?). Finally, because participants were asked the same questions throughout the study, they might answer positively at later study of the study because of anticipation or pressure to conform to what they feel the researcher wants to hear.
I’m interested in finding out why the EDE scores, while they were the same after the intervention for the yoga and no yoga groups, decreased for the yoga group a month after the yoga sessions stopped. This is something that’s confusing me, and I’m not sure what the answer is.
In any case, it is an interesting study and I’m looking forward to future studies with large sample sizes, longer interventions, and adult populations.
Readers, has yoga helped you during eating disorder recovery? If yes, how so? And if not, why do you think it hasn’t?
By the way, the topic for today’s post was suggested to me on Tumblr (so thank you to the person who made the suggestion!). As always, remember that you can leave a note for me in the comments section of the ‘Topic Suggestions‘ page or using the link below. I love reader feedback, links to interesting articles or topic suggestions.
References
Carei, T., Fyfe-Johnson, A., Breuner, C., & Brown, M. (2010). Randomized Controlled Clinical Trial of Yoga in the Treatment of Eating Disorders Journal of Adolescent Health, 46 (4), 346-351 DOI: 10.1016/j.jadohealth.2009.08.007
Thanks for a great post- very important! I’m happy to see it’s getting research attention.
I started treatment for my EDNOS after five years of illness in 2009. The treatment was basically just CBT, and I thought of myself as recovered around autumn of 2011. After a tiny relapse in spring 2012, I’ve been more than fine.
During my treatment I started, by myself and not as a part of the actual treatment, doing yoga. Mostly at my gym where a very sweet young girl was teaching. I liked it and continued, practicing on average 4 hours a week. In September of 2011, I became a fitness yoga teacher myself.
I found that yoga helped me to experience my body in a positive way. The quick improvement of flexibility and strength in yoga made me appreciate what my body can do – and in the long run, that I need to take care of it, not fight against it. Furthermore it became a method of calming myself down when everything was too much and I hated everything; and taking refuge in my body was a critical turning point for me.
I sure hope for more research of this kind! I agree on the amount of yoga – perhaps a solid hour every second day? I guess if it is to help, you need to integrate as part of life and treatment. And if the participants say that they don’t think about weight when doing yoga – give them more of that time!
Also having worked on a voluntary basis with ED recovering people and having known lots of ED patients, it is my experience that there is a world of difference between AN and BN. I don’t know if there’s research out there to back that up, but I’ll have a look later. Anyway, if that’s the case – perhaps researchers should think about having pure AN and BN studies. Perhaps each group respond differently. Idk, it’s just a thought.
Again, thank you for writing about this 🙂
Hi iesteinmark,
Thanks for your comment!
I can definitely identify with this: “I found that yoga helped me to experience my body in a positive way. The quick improvement of flexibility and strength in yoga made me appreciate what my body can do – and in the long run, that I need to take care of it, not fight against it. Furthermore it became a method of calming myself down when everything was too much and I hated everything; and taking refuge in my body was a critical turning point for me.”
For me, that was long-distance running. I loved it so much (do it less now) that I wanted to eat enough to be able to do those long runs. And it made me feel amazing about my body. Though I was at a much higher weight than at my lowest, I think it helped me, as you say, “experience my body in a positive way.” It also made me want to take care of it (because I loved running and the thought of not being able to run was scary.) In fact, when I relapsed and lost weight, I made myself stop running because I didn’t want to harm my body and thought I should only do that when I treat my body well.
Thinking back to this study, though. I think it would be better, or might be better, if they didn’t do an RCT model. Why not see how well yoga works for people who like yoga, or think they might like yoga. I imagine if I was put into the yoga group, I’d be bored and disengaged. I think it will be important to figure out what subgroup of patients benefit the most from adding yoga to their treatment.
There are differences between AN and BN, but a lot of people, myself included, have bounced back between these disorders countless times. I wonder if it would impact whether someone would fare better or worse by adding yoga to their treatment plan. I’m not sure. I agree though, it would be interesting to see.
Cheers,
Tetyana
Did they say what kind of yoga they did? I’ve done some that’s very physically intensive, and some that’s very gentle and spiritual. So if we see a benefit, are we talking about a benefit from physical activity, or mindfulness training?