Why do some people recover anorexia nervosa relatively quickly while others seem to struggle for years or decades? Does it depend on the person’s desire to get better? Their willpower? How much they are willing to fight? Is it just that some try harder than others? Some might say yes, but most will correctly realize that the picture is much, much more complex.
We can spend hours talking about barriers to treatment, but in this post I want to talk about something slightly different, something perhaps that is perhaps less “obvious.”
Suppose a group of girls–all roughly the same age, same illness duration, same socioeconomic background and race–enter the same treatment facility. What determines why some will do well in treatment and continue to do well after discharge, whereas others will relapse immediately after discharge, and yet others won’t respond to treatment at all? We know that catching eating disorders early is crucial, but what else is important?
There will never be a treatment that will work for all eating disorder patients. But some types of treatment will work better than others for particular populations of ED patients. Identifying what treatment approaches work best for what subgroups is crucial if we want to improve recovery rates. In order to do that, we also need to identify what factors are associated with recovery and what factors are associated with increased illness duration, so that we can develop approaches to target specific patients groups.
Identifying prognostic factors associated with illness duration and recovery could have crucial benefits. First, it would help patients, family members, and treatment providers manage expectations for illness duration and plan treatment options. Second, it would potentially assist providers in identifying which patients are at highest risk for developing a lengthy course or chronic illness. Third, it would aid providers in tailoring treatment to target each patient’s individual risk factors for a longer length of illness while also reinforcing the patient’s unique protective factors for recovery. Increasing the intensity or specificity of early treatment for the most at-risk patients could, in turn, shorten illness length or prevent chronicity.
In this study, Stephanie Zerwas and colleagues (2013) identified prognostic factors associated with recovery from anorexia nervosa using a retrospective study design. To be included in the study, women had to have been diagnosed with AN (excluding the amenorrhea criterion), be between 13-65, have had AN at least three years prior to study (this is to reduce likelihood that participants will develop binge eating in the future, because it usually develops within first three years), and have had AN onset before the age of 25.
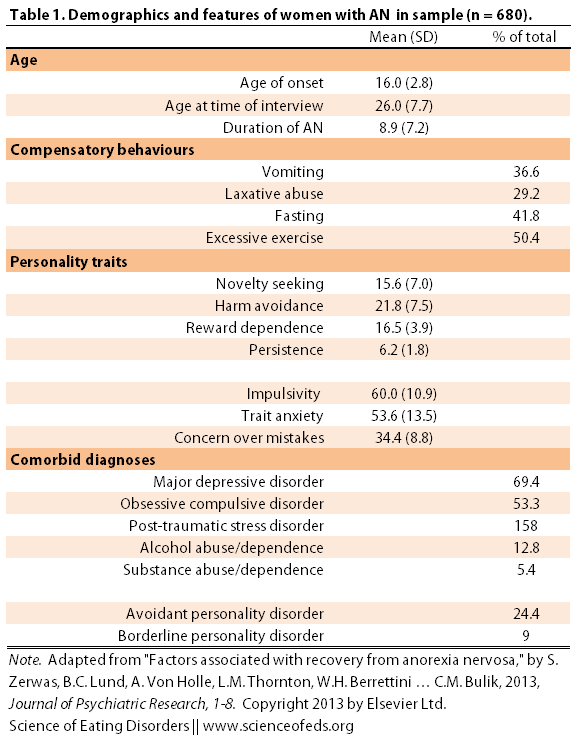
In total, they had 680 AN women from nine different sites across North America and Europe, fill out questionnaires and complete structured interviews on eating disorder history, behaviours, personality and temperament, and comorbid disorders.
In this study, recovery was defined as 12 months symptom free. Of the participants, only 18.1% met this criteria (but they have been recovered for an average of 5.7 years). The mean age of the participants was 26. Below is a more comprehensive summary of the sample demographics as well as the personality traits and comorbid diagnoses:
(Unfortunately, I couldn’t easily find the values for the personality questionnaires for normal healthy controls online, so it is hard for me to get a sense of how these data compare to healthy controls. If anyone has links, please let me know.)
MAIN FINDINGS
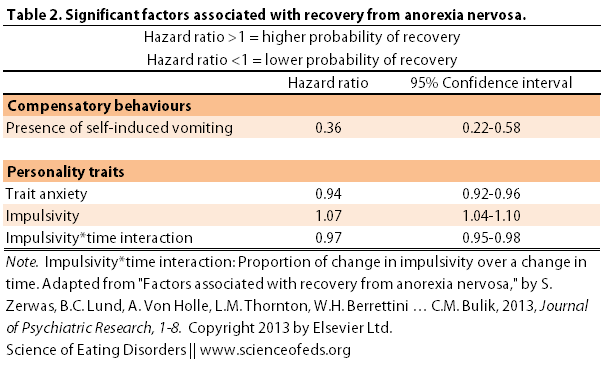
I’m not going to bore you with the statistical models, but long story short, a few predictors of recovery emerged. In the table below, I summarized the factors that reached significance. A hazard ratio of greater than one indicates that the factor is associated with a higher likelihood of recovery whereas a hazard ratio of less than one indicates a lower probability of recovery. (Click here to find out about confidence intervals.)
So what did Zerwas and colleagues find? First, vomiting was strongly associated with a lower likelihood of recovery. Trait anxiety was also associated with a lower likelihood of recovery.
Interestingly, impulsivity was associated with a higher likelihood of recovery, though the relationship between impulsivity and recovery varied through time. Of note, a diagnosis of avoidant personality disorder also decreased the likelihood of recovery but did not reach significance in the final model.
WHAT DOES THIS MEAN?
Vomiting and higher levels of anxiety reduce likelihood of recovery
Although it is not surprising that vomiting and higher levels of anxiety are associated with a lower likelihood of recovery, it is interesting to hypothesize about why vomiting, as opposed to other compensatory behaviours, and anxiety, as opposed to other personality/temperament traits were more predictive.
Though it is unclear, the authors hypothesize that vomiting mt might be “related to higher levels of psychological disturbance seen in individuals with AN and purging.” These disturbances can interfere with treatment.
As for anxiety, food restriction and exercise are thought to have an anxiety-reducing (anxiolytic) effect (I’ve talked about this a lot). The higher the levels of anxiety and the more effective restriction/exercise/purging is at removing the anxiety, the stronger the negative reinforcement to continue using those behaviours to decrease the anxious state.
Moreover, anxiety disorders tend to run in families with eating disorder patients and occur prior to onset of AN, suggesting that anxiety might increase the risk of developing an ED and subsequently decrease chances of recovery. I would also think that it suggests there is genetic overlap between factors that predispose individuals to AN and anxiety disorders. (I’ve talked in more depth about the links between AN and anxiety here.)
What about impulsivity?
What’s more interesting is that impulsivity was associated with a higher likelihood of recovery. You might be wondering what I meant by “the relationship… varied through time.” Zerwas et al. explain: :at onset, impulsivity was positively associated with recovery, but as duration of AN increased, the positive association between impulsivity and recovery declined.”
Previous studies have found impulsivity to be associated with a negative outcome, so the generalizability of the data in this study are uncertain. Is it just fluctuation? Might it be because of the different ways the authors of the studies measured impulsivity?
Fichter et al.’s (2006) measure of impulsivity included ratings of auto-aggressive behavior, shoplifting of nonfood articles, and promiscuity. Impulsivity in the present study was measured with the BIS, which may capture different psychological constructs. Impulsivity as measured by the BIS may be associated with recovery from AN because it tempers the rigidity and intractability often associated with AN and could encourage experimenting with healthier eating behaviors, whereas Fichter et al.’s (2006) measure might more appropriately index sensation-seeking behaviors.
MY OWN UNPOLISHED THOUGHTS…
I thought it was interesting that vomiting was a negative prognostic factors and impulsivity was a positive factor, given that impulsivity is associated with bingeing and purging behaviours. Which led me to think: in this study, the authors largely excluded patients that had binge eating behaviours. Which means that most of the individuals who engaged in self-induced vomiting were not bingeing and purging, they were just purging.
To me, bingeing and purging is very different from purging a normal meal. Anecdotally, I have noticed that those with AN who restrict and purge, but do not binge, seem to be more rigid in their thinking, and often more anxious. Those who binge and purge seem to fare better, overall. (I’m making generalizations and hypothesizing, so please don’t take it to mean that this applies to everyone.) Perhaps in this study, since those who binge/purge were largely excluded, impulsivity became an important variable in predicting recovery, for the reasons quoted above.
Is binge eating a positive predictive factor in recovery from anorexia nervosa? Indeed, is the shift from restricting to bingeing and purging type AN and perhaps subsequently to bulimia nervosa, a positive predictive factor in recovery over the long term? Surprisingly, I haven’t researched this question. I want to say ‘Yes’ but I hesitate because I might be overly reliant on my personal experiences.
As always, it is important to mention the strengths and limitations of the study so that we are careful not to overinterpret the findings. Some strengths: large sample size, strict definition of recovery, multisite study, varied sources of participants (more representative of the AN population as a whole).
There are some weaknesses. Retrospective studies have pros and cons, and one of the cons is that we are generally pretty crappy at accurately describing how we felt and what we thought. There’s also hindsight bias, recall bias, and generally skew events. This is particularly problematic when coloured by malnutrition and malnutrition-induced cognitive deficits. The authors also assumed that participants did not have a period of recovery during the duration of their ED (unless they were the 18.1% that were recovered at the time of the study). Naturally, if this assumption is incorrect, it may pose some problems to the interpretation of the data.
Anyway, I’d love to hear your thoughts! Leave a comment and let me know what you think about these data.
References
Zerwas, S., Lund, B., Von Holle, A., Thornton, L., Berrettini, W., Brandt, H., Crawford, S., Fichter, M., Halmi, K., Johnson, C., Kaplan, A., La Via, M., Mitchell, J., Rotondo, A., Strober, M., Woodside, D., Kaye, W., & Bulik, C. (2013). Factors associated with recovery from anorexia nervosa Journal of Psychiatric Research DOI: 10.1016/j.jpsychires.2013.02.011
Your observations make perfect sense to me. I struggle with AN/purging but have never binged in my life. I am an extremely rigid person and I’ve had anxiety my entire life. I’ve never ever been described as/thought of myself as impulsive. I’m much more compulsive in my behaviors. I actually think it would be to my benefit if I could become more impulsive/spontaneous. Interesting article…I’d like to see more on this.
Yeah, I’m not particularly impulsive I feel either, but I guess more so than someone with just AN-P — but not anything I’d think would be considered impulsive in a non eating disorder population. I started bingeing pretty early on, and purging about 4 years after. But bulimia forced me to not know the calories I was consuming, because I just couldn’t know, it was impossible. When I’d binge but not purge for a while, it forced me to realize that weighing more wasn’t the end of the world. It definitely loosed up the rigidity (though I can quickly fall back to it, to be honest).
It certainly wasn’t a fun kind of spontaneous. I’m much happier being more rigid and structured, but having vacillated SO MUCH between two extremes of being SUPER rigid and unable to see out of it and being ridiculously unstructured and chaotic, I think it has helped me see some perspective and made me MUCH less affected by behaviours on a psychological level. I find that I’m more symptomatic than many people I know who struggle WAY WAY WAY more with thoughts. I’m ridiculously happy with my life right now.
It is interesting. The variability between people is really, really interesting.
I see extreme rigidity, an obsessive-compulsive personality, general anxiety and depression as the primary reasons why, after a 36 year history of restricting AN (no vomiting, or laxative use, but rigid exercising), I am still underweight. I cannot cope with change in ANY area of my life. I never go on holiday, for example, and efforts to spend just one night away from home leave me frantic and panicking. I haven’t a clue why. Goodness, I have tried…. really, really, really hard to expose myself to things that make me anxious, but I become so overwhelmed with change that I feel near suicidal. As I’ve said many times before, my AN is not driven by body image concerns at all, but there have been times when I have feared seeing the number change on the scales because to me this signifies change and the unknown. I score very low on tests of impulsivity…….
Looking at the figures you quote the one that really stands out is the self induced vomiting, which appears to be associated with a 74% lower risk of recovery. I would have thought thought that from the figures quoted anxiety slightly increases the chance of recovery and impulsivity decreases it. Both however by only small but significant amounts. Interestingly both these traits were widely represented in the sample with more than half of those surveyed having these traits, and presumably some both. Unfortunately it does not appear as though this study gives a lot to work on, but at least it is one small step in the right direction.
Ah, I screwed up the table! The 0.94 value goes with anxiety. Off to fix that now.
I have had AN type 2 chronically for about 20ish years (because I had it before then but not clinically, so longer if you counted that as maybe EDNOS?) I did start bingeing and purging in about the 3rd year of constant hospital admissions, but for years before that was mostly AN restricting with a short period of compulsive overeating during a very difficult time of my life. Apart from that period,I’ve pretty much always been underweight, most of the time severely so.
I think one of the limitations of the study is that they don’t include people with AN who binge – because I would have thought that that’s actually quite common? Starvation does seem to be a predictor of bingeing because the body is trying to survive? Or is that actually not accurate? I do think that for them to have created subtype II there must have been a fair amount of bingeing AN people.
Definitely agree that vomiting would be a huge predictor of not recovering – I found that after I finally worked out how to do it, things went to a whole new level of hell. I still say and think that it was like opening the gates to hell and not being able to close them against the tide of what came rushing through. Or like Pandora’s Box where you are better off not knowing what is in there but once you do, you can’t get that lid back on there. As well as bingeing, the main reason I’ve vomited has been to get rid of even the small amounts I’ve ‘allowed’ myself to eat. I’ve also found that physically/medically I got way sicker being anorexic type II than just restricting, because of my tendency to completely go without food or drink unless it’s a binge – and I purge to the degree that I lose weight despite the binges often being calorifically huge. I think it puts my body through a heck of a lot more than when I used to count every morsel I put in because it was going to stay in there. It’s a lot more violent.
I’m not surprised about anxiety either. In the friends I have who are long term AN, they mostly seem to be very rigid in thinking, have obsessive personality disorder or OCD, be perfectionists, and be very controlling – to be out of control or anything less than perfect increases their anxiety. I think for a lot of people too, starvation does decrease anxiety by altering the serotonin levels (I think!!).
I am surprised about impulsivity! I think I would classify as impulsive as I’ve struggled with shoplifting food in the past. I can see why some people might recover from AN if they are impulsive – in my mind, I’m wondering if a lot of those people are the ones who go on to replace their ED with other things eg a drug addiction or alcohol etc?
I think this is a very interesting post and it’s really gotten me thinking. Thank you so much for sharing.
I was wondering, when describing impulsivity they specifically said shoplifting of non-food items.. I have never shoplifted non-food items, it’s always been food, because of the bingeing, and also the ‘missing out’ starvation feeling and the hoarding. It’s never felt anything less than out of control and I’ve HATED it. Even now when I haven’t done it for ages, I think about it and fear it every single day. Is there any reason you know of why they don’t include shoplifting food in impulsivity too? Thank you 🙂
I agree with the limitation of the study because it excluded those who binge afterwards. Even if one has had AN for over 3 years (possibly 4, but I did not become underweight until about 2.5 years into restricting, although I ate significantly less calories the first 2 years when I was actually not underweight yet!), they could still binge afterwards. Not that anecdotal evidence is particularly scientific, but I know that I had AN for 3 years and I started to binge afterwards (still do, I am about 6 months into recovery).
Excluding those who binge afterwards makes it seem like I didn’t have “real” AN because I binged after the 3 years. It makes me a bit angry.
Very interesting. I must admit, I’m skeptical of reading too much into the findings because of the large n and fairly small effect sizes. I know, I know…even small factors that explain some variance can be important :).
Anyway, I was wondering what questionnaire they used for impulsivity and if that has any overlapping variance with measures of cognitive flexibility (e.g. set-shifting) within this population? Considering the focus on “rigid” thinking (I’m certainly a member of that club!), I wonder if there may be some cognitive flexibility factor that may mediate the influence of both trait anxiety and impulsivity on recovery outcomes?
I do not think this is a very good study. I like the numbers they used but still it seems misleading to me. First it was a mail in study. That being it is impossible to back up the facts. Second thier is no metion of socioecnomic factors and or family issues, let alone no mention of race, life stressors, abuse ect. Or other mental illness. To me this study seems to have way to broad of criteria. Yes it does hit the chronic issues of Anorexia but this disease is so multifacited to throughly exam it and put labels to it for research. I would like to see it much more precise. Way to much room for variables? I do love the fact that these studies are being done dont get me wrong. I know this is the way to the answers.
Thanks to Tetyana for her post about the paper. I’m so impressed by your interest in the paper and am grateful to be able to answer your questions about it. Can you guys be my peer reviewers before my next article submission? I really appreciate all of your comments!
First off I want to explain why we weren’t able to look at some important factors like bingeing or treatment history. This paper is based on secondary analyses from a large genetic cohort. The original study was designed to look at possible candidate genes associated with anorexia nervosa-restricting subtype. Often in genetic studies you want to have patients who are very similar to each other (a narrow phenotype) to increase the likelihood you’ll find a genetic marker. So the original study specifically excluded patients who had binge eating or went on to later develop binge eating. This was not ideal for these analyses and I would have loved to have had the chance to examine binge eating. But to paraphrase Donald Rumsfeld, you go into statistical analysis with the data you have, not the data you want or will have.
The large sample size is one of the strengths of the paper. It means we were adequately powered to detect significant prognostic factors. Because we looked at a lot of factors, though, we corrected for false discovery to make sure that significant factors weren’t due just to chance. So the hazard ratios are corrected for false discovery. Another strength is that information about each participant’s eating disorder wasn’t based on mail-in responses. Each participant sat down with a clinician for a structured interview about their unique symptoms during their illness.
I think the biggest takeaway from the paper is that vomiting is an especially negative predictor of chronic AN. I think it might be because it’s doubly reinforcing. First, it relieves that intense anxiety after eating, so allows someone to escape from anxiety. But second, so many of my patients describe the relaxation that they get from vomiting. It’s not just that they are less anxious because the food is gone but vomiting itself is pleasurable. When I looked for data on that though it was hard to find. I had to go back to a Kaye paper from the 1980s to find any description of how vomiting can be relaxing for some patients. As a psychologist, it makes me really watch adolescent patients with restricting AN closely and I give their parents signs and signals of vomiting to watch for, because I worry that if they do start vomiting, the disease will be much harder to shake.
I want to touch base on Fiona’s question about impulsivity as well. It’s important to note a couple of things. We looked at individual differences in impulsivity in this specific group of women with restricting anorexia. We know in general that patients with anorexia tend to be really harm avoidant and not impulsive at all. Although patients who scored higher on impulsivity were more likely to recover, it’s not that they would look impulsive if they were compared to someone without anorexia. It’s just that they scored higher on the measure than someone else with anorexia. Fiona, we used the BIS, not the Fichter measure (the Fichter measure is one that measured shoplifting behaviors, so I can’t speak to your shoplifting question, sorry!). The BIS has three subscales attentional impulsiveness, motor impulsiveness and non-planning impulsiveness. Liz’s comment about whether this is actually tapping cognitive flexibility and set-shifting is great and is something that I wish I had thought of in the discussion section. It’s possible that the BIS, although imperfectly, might be tapping some of that dimension. The way I thought of it was that it’s measuring the willingness to attempt something new which is so necessary when your mind is trying to convince you that you’re safe at a low weight and eating is too risky.
This paper will ultimately help us define trajectories (the unique courses) that people take to recovery or to continued illness. Trajectory studies will also help us figure out whether timing of behaviors or stressors (including traumatic events) also predict recovery and can help us steer someone on a recovery course.
Thanks again to Tetyana! Happy to answer any other questions! Really grateful to my co-authors (Ann, Laura and Cindy) as well and it’s nice to know that Tetyana’s post means that more people will know about our findings.
My word, is this a fascinating post. I too wonder, as Tatyana mentions, if an “evolution” from purely restricting anorexia to anorexia-purging type…and then possibly bulimia nervosa…might indicate an “overall positive” indication of recovery “down the road”. Does this indeed indicate a certain “opening”of the spirit..or relinquishing the perceived “control” of the body and mind toward eventually accepting nourishment? I say this because, after ten years of purely restrictive anorexia, I have experienced severe bingeing episodes followed by “thorough” purging due to some bizarre inner, animalistic “need” to consume and consume after extended periods of eating very, very little. I have absolutely zero control over these occurences. It’s as if a “switch” goes off in my head and I literally grab everything I can find. I have actually torn off lettuce or cabbage leaves in supermarkets, broken off carrot tips, helped myself to one or two kumquats, and literally shoved them into my mouth. This kind of behavior is new and frightening. Yet, I wonder if this marks a certain relinquishing of a very strict attitude toward self-nourishment. I do, so direly hope that it is an indicator of a exit from the hell of anorexia…”down the road”. Excellent post, excellent comments…as usual.
Whoops…forgot to inquire about outcome prognosis with relation to age? It appears that my age bracket was represented in this study (I am 52…) but also noticed that late on-set scenarios were not included. Were the recovery percentages very different for the older as opposed to the younger participants?
This is an interesting article. I myself completely recovered from anorexia. I suffered for a 12 years in total. I have an academic background and worked as a counsellor and social work manager in between two bouts of anorexia. My second battle against this terrifying disorder almost cost me my life. I am now attempting to help others who have An Eating Disorder through my own counselling clinic that is located in Derbyshire UK. This area does not have a single specialist eating disorder counsellor either in the NHS(free healthcare)or in the private sector. I feel that the one facet of an eating disorder that unifies all sufferers is the eating disorder “voice” that everyone has to some degree. Here in the UK there is a complete lack of research/ understanding to this element of one eating disorder. It is my contention that unless this “voice” is initially recognised and then dealt with then the eating disorder will remain in some form.
The anorexic voice drives and maintains the disorder to such an extent that the longer this part of the disorder remains then the more likely it is that the patient will never fully recover. As a postgraduate student at Edinburgh University I studied psychology where there was a lot if work done into mental illness. I found that academics and healthcare professionals do not understand the nature of this voice. It not a psychosis and cannot be treated by chemical interventions. That factor is sufficient to send the healthcare professionals running for cover. Psychiatrists have significant difficulties treating any mental illness that they can not treat with medical.
The main psychological interventions here that are provided free by the NHS are almost entirely dependant on CBT. Once again experience has shown me that this approach rather than help alleviate anorexia, it actually strengthens and reinforces the condition.
This approach is too directive and judgemental in my opinion. It’s starting point is that there is a dysfunction of thinking etc that needs to be corrected. It aims to correct behaviours by the good old Skinnerian tactic of reconditioning. After all CBT is just skinner rebranded. So when an anorexia is told that his/ behaviour is faulty(or however the therapist describes it) the anorexic voice is immediately strengthened and started to fight back. This approach does not recognise that there is even a thing as the anorexic voice. Ideas such such promoting positive reinforcement have no place in the treating of an eating disorder. Enforced completion of food diaries is a pointless exercise as most anorexics will not tell the truth when they complete them. The voice is so powerful that it has problems in convincing the sufferer to lie. Counselling an anorexic is never easy as the nature if the illness makes the sufferer resistant to treatment. But unless this voice is controlled and eliminate then I believe that the condition will continue in form within the patient.
Early diagnosis and treatment is essential. The UK has an appalling record of treating anorexia. In large areas of the country there simply is not any treatment available. Very few therapists actually have had an eating disorder. The NHS will not employ professionals who have had a mental illness. Also cost is a significant factor here. There are always places available for in patient treatment at eating disorder clinics because the funding authorities will not find the treatment. NHS clinics are always oversubscribed because authorities prefer to keep,the funding within the state sector. This is a narrow minded view that ignores the fact that the longer a patient remains untreated the more it costs to treat them in the long term
I do have radical views on the treatment of eating disorders. These are based on my academic, professional and personal experiences. I have so far been unable to convince any NHS funding bodies to expand their services to include the private sector. They have acknowledged that there is a need for specialist services, however they refuse to take the next obvious step to actually set up services. The basic service here does not treat anyone unless their BMI is 15 or less. This tells the anorexic that in order to receive treatment that they have to lose weight. This is an appalling approach to treatment. When someone does qualify for treatment the service does not off any counselling at all. They concentrate of refeeding and ignore the psychological side of the illness. Essentially in the UK anorexia is recognised as a mental illness and treated almost entirely as a physical illness. Until this anomaly is recognised then the prevalence of anorexia will increase and Fewer patient will recover.
Wow! It was really interesting to read about this perspective on treatment of ED within the UK. My personal experiences align with yours: I had to get rid of the “voice” in order to stop the disorder. I was completely aware of everything I was doing to damage myself, but I couldn’t truly quit until I started to develop an intrinsic sense of self worth.
While this is my experience, I’m not sure if others have struggled with the same lack of self-love in their ED. I also find that this low self-efficacy seems to be more highly correlated with anorexia nervosa than other ED?
I’m curious, What specifically is “the voice”? Is it a self-worth thing, or something else?
What indeed is the “voice” We all have an inner voice. In many ways it is just a reflection of ourselves. Generally, most people are able to turn their inner voice on and off as and when they choose. In my experience the anorexic voice is entirely different in the way that it controls the anorexic rather than the reverse. It is there in ones head 24/7. It directs and controls the sufferers lives. One moment it’s your best friend and then next in an instant it becomes your worst enemy. I realise that I am making it sound like a real entity. Well, to the anorexic, it is a real entity. It is insidious in nature and will do whatever it takes to survive.
As I said earlier this is not a psychotic voice outside of your head. This is an equally terrifying voice inside your head. It is your voice, but it is not a voice you can hear. It is just the thoughts of the voice you hear. It is impossible to quantify this voice and as you can see from my vague answer it is also impossible to explain. All i know is that you will find this voice exists in the head of every single anorexic and it will make theirs lives an absolute nightmare.
As far as I am concerned the major determinant of recovery is how far we gain control of this voice. Many chronic sufferers will learn to live with their anorexia rather than actually beat it. This is an uneasy compromise where serious relapse in always possible.
I am a published researcher and I would sincerely like to look into this completely overlooked “phenomenon” I would suggest that a longitudinal study is urgently required here to at least address and acknowledge the voice.
We need to question how effective in-patient treatment is beyond simply refeeding anoroxics to a safe BMI. We need to look at the return rate of sufferers to hospital. Think of returning patients as a form of mental recidivism rather just a relapse into old habits.
How many sufferers actually leave hospital free of their anorexia? How many patients even get asked about their anorexic voice?
There needs to be significant work done in many areas in order to assess the true impact of treatment. patients need to be tracked after discharge and where they are willing I would enlist a cross section of them in a long term study to really see how many of them are free of the anorexia and how many just learn to live with it. It is almost impossible to live harmoniously with an eating disorder. So those who choose to live with it are choosing a life that the majority of the population would find intolerable.
I feel that here in the UK that the anorexic community of being failed by a scared and indifferent healthcare service that doesn’t ask the right questions because it simply does not want to hear the answers.
When the psychiatric profession does not have an answer then it does nothing. And the longer we avoid the questions then the higher the financial costs will be in the long run ad the costs to the individual sufferer are incalculable.
I’m not sure that it’s just an ‘anorexic’ voice. I’m recovered from anorexia, which in my case was, I think, secondary to anxiety, and still struggle a lot with a hyper-critical inner ‘voice’ that I can’t figure out how to switch off. It had and continues to have an incredibly negative effect on my life.
I agree about the problem with over-reliance on CBT. I’ve had extremely negative experiences with CBT — for me, it’s been either not helpful or actively harmful; it basically treats black-and-white, shame-based thinking with more black-and-white, shame-based thinking.
Please follow and publicise my website and blog at
derbyshirecounsellingservice.com
and
http://kindofblue62.wordpress.com/
I am trying to reach out and help counsel other eating disorder sufferers. Sadly in the UK it is very almost impossible for private therapists/specialists to actually get the healthcare establishment (NHS) to pay any attention to us. So I need all of the support I can get to really make an impact on the community.