The experiences of siblings of individuals with eating disorders has received relatively little space in the academic literature to date. Several studies have revealed the disruptions in family life that can occur when a child has an eating disorder (for example, see Hillege, Beale & McMaster, 2005 and Perkins et al., 2004). On the other hand, some studies have shown that siblings of patients with chronic illnesses have both positive (personal growth, responsibility, increased empathy) as well as negative (worry, fear, resentment) experiences.
However, few studies have explored experiences of male siblings, older siblings, or siblings of adolescents with eating disorder not otherwise specified (EDNOS). Consequently, to help fill this gap, Areemit, Katzman, Pinhas & Kaufman (2010) conducted a mixed-methods study looking at experiences and quality of life among siblings of adolescents with eating disorders.
Twenty siblings were recruited from The Hospital for Sick Children in Toronto. All lived with their ill sibling (hereafter AED for “adolescent with an eating disorder”, as they were called in the study), who had been diagnosed at least 3 months prior, were between the ages of 10-18, and had a family doctor. The mean age of the siblings was 13.5, with 10 and 16 being the youngest and oldest ages, respectively. There was a mix of older, younger, and twin siblings, with 30% brothers and 70% sisters. The majority (70%) of AEDs were diagnosed with anorexia nervosa and the remaining 30% with EDNOS.
Siblings completed a number of self-report questionnaires aimed to gauge their quality of life (Pediatric Quality of Life Inventory 4.0 Generic Core Scales), their experiences in general (General Assessment Questionnaire), and their eating attitudes/screen for an eating disorder (Eating Attitudes Test). Additionally, siblings who wanted to continue with the research were invited to participate in a focus group; 10 siblings participated in this group.
The authors used Corbin & Strauss’s (1990) grounded theory for qualitative analysis and checked their results with some of the siblings.
WHAT DID THEY FIND?
QUANTITATIVE RESULTS
The quantitative data revealed relatively little; keep in mind that 20 is a very small sample size for a quantitative study, and allows for only weak and tentative conclusions. Nonetheless, the descriptive statistics the authors calculated (the majority of which I described above) makes interpretation of the qualitative results quite interesting.
In terms of questionnaire results, the authors noted that 80% of siblings reported a decline in quality of life. However, none of the siblings met the quality of life survey’s cut-off point for “risk of impaired quality of life.” It is likely that more interesting and assertive quantitative results would have emerged if the authors had used a larger sample.
QUALITATIVE RESULTS
Overall, the siblings described their lives in conflicted ways. The key themes reflect the duality in their lives:
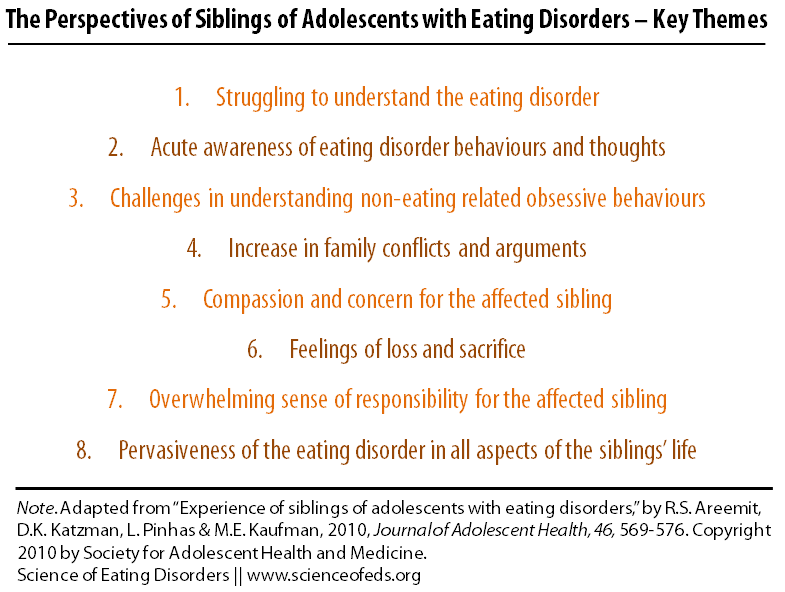
1. Struggling to understand the ED
Siblings were not always given information about their sibling’s eating disorder and reported feelings of confusion, anger, and frustration. They reported different understandings of eating disorder etiology, sometimes fluctuating between feeling as though the sibling wanted attention and at the same time seeing the eating disorder as something over which the AED had no control. For example, one sibling said:
Yeah it’s like, when people are saying ‘what is wrong with those people; why don’t they just control it’, you feel kind of defensive but you’re thinking the same thing.
2. Acute awareness of ED behaviours and thoughts
Among the changes in siblings’ lives was the development of a greater awareness of eating attitudes and behaviours surrounding them. Though siblings did not see (or admit to) changes in their own eating overall, some reported having “experimented” with the AED’s eating behaviours. They also noted being more sensitized to the social context surrounding food, dieting and fat talk (from the AED or others).
One sibling commented:
I never lend her any of my clothes any more because she’ll say, ‘I couldn’t wear the clothes because it was too big for me, it was just too big for me’. I’ll be like, okay, ‘You don’t need to tell me that three times. Yes, I’m bigger than you’.
3. Challenges in understanding non-eating related obsessive behaviours
Interestingly, and related to the first theme, siblings struggled most to understand behaviours that were not related to food. Behaviours that seemed to stem from comorbid conditions (e.g. obsessive-compulsive disorder) made siblings feel more alienated, as they did not seem to be clearly linked to the eating disorder.
4. Increase in family conflicts and arguments
Family conflicts, both between parents, and between the AED and various members of the family, were noted to have increased, according to siblings. They suggested that these fights often centered on negotiation, lies, and secrecy, and they seemed unfair to them. In conflict situations, siblings also felt torn between loyalty to parents and to their sibling. Participants also reported being fearful of fights breaking out over meal times. However, despite this increased familial conflict, some siblings also talked about the eating disorder having brought the family closer together.
5. Compassion and concern for the AED
Worry and concern for the AED were common among siblings; many feared for their sibling’s life and long-term health. This was also coupled with a desire to safeguard the AED from the judgment of less compassionate others. For example, one sibling noted:
It’s so easy for people to say ‘[you should] try not to think about it, but you can’t not think about it. How can you not think about it when someone who you love is just suffering?
6. Feelings of loss and sacrifice
Despite their compassionate outlook, siblings also described losses, such as loss of personal identity, closeness with the AED, and a “normal childhood.” This was sometimes articulated in terms of appearing (or fearing that they might appear) to be just the sibling of a person with an eating disorder. This led some to isolate and become more private, or to take on the identity of “the undemanding, silent child.” The process of shifting identity was not uniformly negative, however, with some siblings noting positive changes, particularly the development of better self-understanding.
7. Overwhelming sense of responsibility for the AED
Siblings’ sense of responsibility for the eating disorder seemed to differ by age. The authors note that older siblings reflected on things they might have done that could have contributed, whereas younger siblings feared doing the “wrong thing” in the future. For example, one sibling said:
Sometimes I blurt something out by accident, not knowing what it means, without thinking it straight, and then she gets the wrong idea. So, sometimes I feel like it’s something I did wrong.
Another:
I’ve always been like that; I’m responsible for everything. I always thought back to all the things that I ever said (sniffling) ‘am I like a bad sister?’ Which I know I have been a good sister but (crying), I blamed myself for that. I don’t know, I just thought ‘what did I say?’ or ‘what did I do that made her feel she wasn’t good enough?’. Maybe I should not have said, ‘those pants are too small’.
Again, the issue of mixed loyalty resurfaced, as siblings were unsure whether to report to their parents when they saw the AED engaging in eating disordered behaviours. Many felt that they should help in managing their sibling’s ED, for example through supervising mealtime.
8. Pervasiveness of the ED in all aspects of the siblings’ life
The eating disorder impacted siblings’ lives in a number of different ways, and in different areas of their lives. Siblings reported adapting to these changes and integrating the differences into their lives by taking on new roles and/or responsibilities.
IMPLICATIONS
Overall, this study highlights how eating disorders can come to have huge impacts on siblings, as well as families in general. While I wouldn’t call this a unique finding in the vast eating disorder literature, the particular experiences described by siblings help to shed some light on areas in which interventions or support might be most useful. Based on the qualitative results, providing siblings with information and support that would help them to navigate the at-times confusing experience of living with an individual could be a helpful approach.
Of course, more research is needed to increase the generalizability of these findings. As the authors note, the sample included in this study all elected to participate and the focus group participants were particularly eager to share their experiences. Finding a way to include siblings who felt more disengaged would be extremely interesting in terms of reaching the voices that are harder to hear. Some larger studies in the quantitative realm might also illuminate potential differences in experience between genders, older and younger siblings, and siblings in different types of households.
Searching for the anecdotal, I’m curious: Have any readers talked to their siblings about their experiences? My own brother is a closed book and we also lived separately for much of the time I was actively symptomatic so I still have no idea, unfortunately, what it was like for him to have a sister with an eating disorder.
References
Areemit, R.S., Katzman, D.K., Pinhas, L., & Kaufman, M.E. (2010). The experience of siblings of adolescents with eating disorders. The Journal of Adolescent Health, 46 (6), 569-76 PMID: 20472214
I’ve found this extremely interesting. As a Transactional Analyst, your brief examples around sibling experiences jump out as being a power struggle within the sibling dynamic with the non- eating disordered siblings being left confused about what is going on. A great angle to be explored and I hope you continue with this for longer. Please email me any other responses you can share.
Thanks for commenting, Patricia. I wasn’t sure what a transactional analyst was so I looked it up, and I can see why you’ve honed in on the power struggle and the sibling dynamic. Have you encountered this in your practice?
I am not personally conducting this research, I just wrote the post about the article, so I wouldn’t be able to send along any responses, but I encourage you to read the full article if you’re interested in reading more (it has more quotes and more detailed info).
This was an interesting read. Having had a sister who struggled with an EDNOS, it is true I think that life was different growing up. I think that it made me hyper aware of the obsession people had on their looks. It is sad that society pushes a certain look to such an extreme that one can get wrapped up in obtaining it!
In my psychology class we are reading how certain things can trigger early menarche. Having been only eleven and a half when I started, it makes me wonder if it could have been due to the stress we all went through at the time. It is said that many factors can play a role, like: biological programming, nutrition, health and a sturdy home life. All of these were normal for me. The only thing really out of wack would have been my sister having an EDNOS. Maybe, someone should look into that as well.
Thanks for the comment, great to hear from a sibling! I think it is interesting that you can relate in particular to the hyper-awareness of image-oriented culture. Some of the subtleties of environmental triggers and obsessions can go unnoticed by those who haven’t experienced disordered eating firsthand, such as through having a sibling with an eating disorder. It can be extremely difficult to recover in the society in which we live, when everything you need to do to recover goes against the (at times tacit) social norms that circulate. As I’ve noted before, these factors don’t cause eating disorders, but they certainly don’t make life and recovery any easier.
I definitely think that it would be interesting to look more deeply at impacts on siblings, including physiological changes, as you suggest. Stress can be extremely impactful, physically and mentally. I hope you and your sister are doing well.
Really interesting and I hope to see much more research involving this topic. I have an identical twin sister who lives in the U.S. while I live in Europe presently. While we attended universities in the US..at different colleges, we both later “shared”/discovered that we had simultaneously, privately..dealt with bulimia nervosa throughout the undergrad years. She recovered post-university…and I thought I had recovered “for good” as well…But strangely, after a twenty-year reprieve…ED re-surfaced as anorexia nervosa for me which I have been battling for nearly ten years.
This upsets my twin, and she wonders why I cannot seem to vanquish the ED this time and she is perplexed as to why she apparently has been “spared” and why I can’t “get over it” as she has…since we’re of the same genetic make-up.
Thanks for your comment, Donna. Your story is fascinating- your shared and different experiences with your twin must make for some very interesting (and as you mention, not always easy) dynamics going on there. Thanks for sharing! I, too, hope that there is more research involving the topic, it has really sparked my interest.
Epigenetic changes that accumulate throughout lifetime are quite significant that gene regulation and expression (which genes are “turned on”) can be quite varied even among identical twins. That’s (at least in part) because the environment (i.e., life events, social network, etc) can be very different.
This paper made a lot of splash when it was published.
Here’s a good image to show the differences between two chromosomes that accumulate in identical twins throughout age:
http://php.med.unsw.edu.au/embryology/index.php?title=File:Epigenetics_-_monozygous_twins.jpg
“Monozygous twins share a common genotype. However, most monozygotic twin pairs are not identical; several types of phenotypic discordance may be observed, such as differences in susceptibilities to disease and a wide range of anthropomorphic features. There are several possible explanations for these observations, but one is the existence of epigenetic differences. To address this issue, we examined the … differences in [epigenetics] of a large cohort of monozygotic twins. We found that, although twins are epigenetically indistinguishable during the early years of life, older monozygous twins exhibited remarkable differences in [epigenetic changes] affecting their gene-expression…. These findings indicate how an appreciation of epigenetics is missing from our understanding of how different phenotypes can be originated from the same genotype.”
Thanks for the info, Tetyana- I find the idea of epigenetics interesting but don’t know much about them and the mechanisms through which they work.
There are a few, including DNA methylation and histone modification, which seem to be the most studied. They are essentially just ways of modulating gene expression. For example, DNA methylation just means adding a methyl group (to cytosine or adenine nucleotides) which can essentially silence the gene expression. I know the genetics side more than the environment side of the coin. Technically, these changes are only epigenetic if they can be passed down through generations, but people seem to refer to these changes as epigenetic regardless of that… probably because it is a trendy buzzword.
I’m new to the site and am loving it so, thanks to every one! This caught my interest for two reasons. (1) I was 12 yo when diagnosed and had a 7 yo sister….I always wondered if the distance between us started, or was triggered by, what her experiences with my AN were. Since this was back in the early 80’s they weren’t sure what to do with the patient, let alone siblings. I so hope that this research continues!!
(2) Being 45 yo, still struggling with AN (and permanent disability from diseases that I’m sure resulted from all these yrs of restricting) and having a teenage daughter. (I was able to have a child after 6 mo of constant treatment and to this day the family refers to her as a miracle *sniff sniff*lol) Obviously I adore my daughter and from the beginning of her life I worked very hard to be open about eating disorders and my experience with them. As she has hit the teen yrs, I know the education I gave her has stuck….she watches me like a hawk and is starting to demand I get help. I guess my point is that I have apparently avoided thinking about any damage I am doing to her, by restricting actively. It would be interesting to see if children’s perspectives would be similar whether a sibling of an AED or the child OF an adult with an ED.
Thanks for your comment, Wendi. Interesting observations about both your relationship with your sister and your fears about your interactions with your daughter. If I recall, there is a small body of literature surrounding parents with eating disorders and the perspectives of their children, but don’t quote me on that- I will look into it; maybe there is an interesting post to be written about that!
Really…currently relating to Wendi’s comment…I am truly concerned as well with the effects my current phase of hard restriction is having on my off-to university daughter. She seems afraid/reticent to begin her new life away from the family nest…and I feel immense guilt about her anxieties…for I fear she “fears” for me.
Thanks for commenting, Donna. I think it is important to avoid taking a self-blaming stance on your daughter’s anxieties about going away- while it could certainly be true that she “fears for you,” it is also totally “normal” (whatever that really means!) for young adults to be anxious about starting a new life away from the family nest. I think it is really important to avoid the self or “mother-blaming” stance in eating disorders in general- there are a myriad of bio-psycho-social factors that play into individuals’ development, and into the development of eating disorders. For too long, the study of eating disorders focused on blaming the individual, and more complicatedly, in this case, on blaming mothers and families, which is why I think it is extra important to avoid doing this, if possible, because it certainly isn’t your fault! Of course, I am not a therapist/counsellor/psychiatrist, so if you are really feeling fearful about this it might be a good idea to check in with a professional about this. I wish you both the best of luck!
Thank you so much for your kind, wise words…for they “encourage”..truly so…at this very moment.
I do plan on tackling these issues of self-blame…punishing myself for being a NOT perfect Mom (although I SO wanted to be)in hospital when I return home post-vacation. I grapple with extreme guilt and issues related to sending off a daughter to university who is not feeling “good in her skin”…having gained much weight as I got sicker…seemingly vicariously eating/nourishing herself “for me”. I feel such the failure and so responsible, despite knowing that there were factors “beyond my control” in this horrific malady. Again, thank you for gentile, helpful words!