A few weeks ago, I asked SEDs readers a bunch of questions about their experiences with an eating disorder. Then, pretending to be a qualitative researcher, I went through the answers to see if I could find trends. I blogged about people’s responses to the first half of the question here; this post will be about the second half of the questions. (Here’s a ED survey results – Parts I and II to the pdf with all of the raw data).
Please note that this analysis was not rigorous, so in grouping and identifying themes (or how many times a theme/word was mentioned), I will use words like “approximately.”
[The breakdown for the last half of the respondents is:
6. What are characteristics of good eating disorder clinicians?
By far the two most comment themes, mentioned ~13 times each were “understanding” and variations of “willing to challenge,” “confront,” and have a “no bullshit” attitude. Other qualities mentioned were patience, good listening skills, nonjudgemental, empathetic and compassionate, not dismissive, patronizing or condescending, and firm but flexible.
Two individuals mentioned the importance of understanding intersectional issues and the complexity of body image issues. A few mentioned having a good sense of humour and not giving up hope. Interestingly (for me, anyway), four mentioned self-disclosure, not necessary of ED issues but something that indicated to the patients that the therapists could relate.
I believe that working with eating disordered clients is all about striking a balance between compassion and toughness. I appreciate therapists who can make me feel understood, validated, and valued… while still calling me out on my bullshit.
Not patronizing, not boxing people in, not demeaning, not deciding that someone is sick and can’t improve, good at listening, not making 100 triggering comments.
Approaching the person properly, based on their age, gender identity, etc. Recognizing the patient’s individuality and tailoring treatment based on what works best for them, not based on what a textbook says ought to work. Being understanding and not dismissive of the patient’s fears.
Thinking about how I’d answer, I would say listening skills are really important. I don’t think understanding is always necessary; but listening and validating your feelings in a non-judgemental way is paramount. Not boxing you in, not making assumptions, and trusting your experiences and feelings are all necessary traits, in my opinion, anyway.
7. What is the most helpful thing a physician/therapist/healthcare worker ever said to you?
Responses to this question were wide and varied, and I couldn’t really find common themes. Although a lot of the statements individuals found to be helpful expressed understanding/nonjudgemental attitudes and many comments were geared toward helping individuals envision a life outside of the eating disorder.
My therapist in day treatment told me that I needed to start getting pissed off at my eating disorder. I did, and I greatly accredit that advice to why I’m still alive.
I’m not mad at you. I really believe that you were doing the absolute best you could in that moment.
Consider this a trial period. You can always go back to your eating disorder if you hate it.
It’s okay to not be okay. You’ll get there one day.
When you look into the mirror in five years, who do you want to see looking back at you? Start becoming that person today.
Reading the responses to this question was interesting as I can imagine, personally, finding some of those comments patronizing, off-putting, or just unhelpful (though not really any of the ones I quoted above). This really points to the fact that we are all different and that different therapeutic approaches work for different people.
8. What is the most helpful thing a family member, friend, or partner ever said to you?
Contrasting the diversity of the responses to the question above, the responses to this question were quite similar: “I love you”, “You are strong,” and “I’ll always be here/listen to you” were extremely common. Here’s a tiny sample of some responses that I particularly liked (they were all great, of course!):
So many people looked at my ED as something I should be able to control, so it took me by surprise when my first partner while in recovery told me how sorry he was that I had been so sick. The lack of blame was comforting.
One thing comes to mind. My best friend told me that she felt like she lost her best friend when I relapsed. I was pretty deep in my eating disorder at the time, and that simple sentence reminded me that I was not the only victim of my disease.
Just because I don’t understand doesn’t mean I don’t love you. I will always be here, and I am always proud of you. – My Dad
My boyfriend . . . told me that he felt as though everyone in my life . . . “already tells me what to do” and that “he doesn’t want to be one more person trying to control me” that he’d rather “be there so I had someone to listen to but wouldn’t give advice”. I think that’s all I’ve ever wanted is someone to care and listen, without judgement.
9. Was there anything that have been told during recovery/treatment (from family, friends, partner, or clinicians) that was really UNHELPFUL (but was probably said with good intentions)?
The usual “but you look so healthy!” and “but you are so skinny!” and “you just need to eat and not throw up” were common answers to this question. The “you’re too smart for this” was also one I’ve gotten many times before.
Thankfully my doctors have been excellent and they haven’t said anything unhelpful or hurtful. From non-professionals it’s the usual crap. . . probably the worst thing was, when I told my brother that he couldn’t force me into a treatment program because I am an adult, he said “You haven’t behaved like one.” Like my ED was something childish, like refusing to clean my room or something. Just another example of someone viewing an ED as something you choose to engage in, rather than a disease you suffer from.
My best friend told me she was “offended” by what I was doing because she is raising a baby who has had to overcome a tremendous amount of obstacles in his short life and I was just “choosing” to throw mine away.
I hear from treatment people and friends: just let it go. If I knew how to do that I wouldn’t be in this position.
These responses in particular sum up a lot of what was echoed in the answers:
Anything about weight, not needing to gain weight, you look fine at the weight you are at: at any weight. When underweight makes you feel guilty to gain, at a “normal” weight makes you feel like you shouldn’t have a problem. Any stupid comments about food. “You don’t look like you have an eating disorder”
1. You’ll never get fully better; anorexia is just something you’re going to have to manage. 2. As long as you get to the minimum healthy BMI that’s fine; you don’t need to gain anymore or try harder to eat. 3. Everyone worries about weight and counts calories; that’s not something you have to try to change. 4. Why don’t you do [specific exercise type]; that will make you feel better. 5. [When weight-restored but still really sick] You look fine, I don’t think you need to see a therapist/dietitian/I don’t think you have an eating problem anymore/etc. 6. Don’t worry, we won’t let you get fat (like getting ‘fat’ was the worst thing in the world and all the clinicians would be watching and judging me if I gained more than they thought was necessary) 7. Oh so many more! but I don’t want to spam.
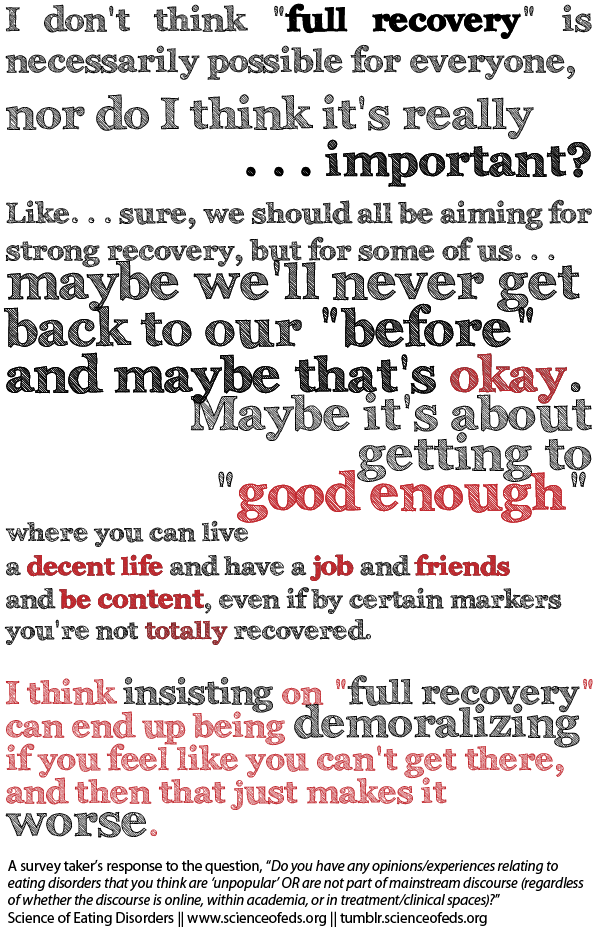
Interestingly, I’ve spoken to several people (all adults who’ve had EDs for 10+ years) who found that being told that AN was just something they’d probably just have to manage to be a huge relief. I think they felt they were no longer under all this pressure to achieve full recovery and they could now finally focus on getting better/improving at their own pace (or to a point that was good for them).
10. What role has your family (or friends, or partner) had when it comes to your eating disorder? Has it been positive, negative, neutral? How so?
The responses ranged from “neutral,” “non existent,” “positive,” “negative,” to “they don’t know.” Here’s a snippet of some of the responses:
My parents’ help is mostly financial. I could not have stayed in treatment as long as I did without their help, and I am incredibly grateful. But my best friend is the one who really keeps me accountable. She isn’t afraid to ask me questions even when she knows the answer won’t be good.
My family either completely ignored it or were pushy (expected me to recover in a week). My partner was incredibly supportive, listened to my issues, tried to support me as best he could and made an effort to understand me. Friends completely ignored the issue, which left me feeling angry and isolated.
My family has had mostly negative roles. They tend to dismiss my struggles and are very triggering in their behavior and talk about food and their bodies.
Unless I’m hospitalized, my family looks the other way. Can’t acknowledge what they don’t want to see.
My family has been integral. They have supported me, pushed me, fed me, held me. The friends I made in treatment have been my lifeline – I have heard horror stories about relationships made in treatment being triggering and toxic but the women I met have held me up and encourage me every day. Also, my horse has been a life saver.
I wonder how these responses change over time — what if I were to poll the same individuals in 5, 10 years? What do you think? How have your feelings with regard to the effect your parents, friends, and partner(s) had on your ED changed over time?
11. Do you have any opinions/experiences relating to eating disorders that you think are “unpopular” OR are not part of mainstream discourse (regardless of whether the discourse is online, within academia, or in treatment/clinical spaces)? If so, what are they?
I think ALL of the responses here are worth a read (although this question did get misinterpreted a few times but that is 100% my fault with respect to the wording). I love a lot of the responses to this question. So, seriously, go read all of them (and add your own in the comments!):
I really hate the idea that recovery is wonderful and rosy and sunshine and rainbows. That’s not to say I don’t think people should recover, I just think that there’s a lot of misinformation and naiveté surrounding it. As far as I can tell, recovery really sucks for the most part. It’s everything you don’t want to do and everything you don’t want to deal with and it fucking HURTS. Eventually (hopefully) it does get easier and wonderful and whatever, but initially it’s not the paradise its painted as.
The whole idea that a “full recovery” means never thinking about or questioning food/exercise. I think that there are standards to which people in recovery are held that are unrealistic and that go against the gain in popular health promotion discourses. To expect that someone who has had an eating disorder will suddenly be able to forget how many calories are in a muffin is, frankly, ridiculous. To say that we are settling for “less than” if we do anything that could be taken as indicative of “remnants of” an eating disorder (for example, continuing to follow a meal plan or refusing a donut when it is offered at some random time) is extraordinarily belittling.
Eating disorder ‘prevention’ campaigns may be dangerous, especially if they mention behaviours / methods / techniques. I began restricting before I knew what EDs were, but I’m sure I wouldn’t have tried purging if I hadn’t heard about it as a method of weight control.Exercise (and I mean fairly strenuous / intensive exercise) has been a really positive tool in helping me eat more and feel more positively towards my body. I enjoy seeing what it can do, and am willing to eat enough / more so that I have the energy and strength to exercise. It also gives me more definite hunger cues.
I don’t believe that calorie counting is inherently disordered. I’ve been out of intensive treatment for a couple months and I still follow a calorie-based meal plan. I definitely don’t look like a “normal” eater yet, but if calorie counting helps me maintain my weight and health long enough to retrain my brain so that I can eat intuitively without restricting, I am okay with looking weird for now! It’s tricky and controversial because for me and many others, calorie counting can be disordered too.
This is one that I could probably relate to the most, personally (though I seriously could relate to most of them in some way):
Lastly, I asked participants to “share anything else” they’d like me to know.
Here are some messages people shared:
Eating disorders are EXTREMELY prevalent in the trans male community.
Positive affirmations have helped me in more ways than any other coping skill!!
This may sound a little stupid, but one of the small factors that exacerbated my disorder was anime-related body image. There is lots of literature about the fashion industry/generational shifts in ideal beauty and stuff affection body image, including Disney princesses, but I’ve seen little to nothing about body image issues associated with animation outside of Disney, especially anime. Don’t know, it’d just be interesting to know if anyone else mentions Sailor-Moon-thigh-envy in their responses.
And finally:
Any information sharing about people’s experience of EDs will help those that suffer from them feel less alone.
I agree! Which is why I did this and I will do more surveys like this in the future! I hope this has been helpful — feel free to share your experiences in the comments below (remember, you can be anonymous and not enter any information, or use a pseudonym).
I’m really happy that you did this. I agree with the last comment that sharing experiences helps people feel less isolated. If you plan to do another, could you consider asking a question around having an ED ‘voice’? I personally have always felt the eating disorder thoughts to belong to me – just a rather negative / self-hating side of me, but find myself using the idea of an ‘ED voice’ more in therapy etc as it seems to fit more with how some clinicians conceptualise EDs (how many times have we heard the phrase ‘that’s just your eating disorder talking’). But yes, thank you for putting people’s experiences out there.
Great idea! I will add that question to the next survey!
Have you seen Andrea’s blog post about this (‘ED voice’)? Here’s the link. A few people (myself included) shared their experiences in the comments thread. From the comments, it seems some found it helpful at first and less so later and others the were the opposite. (Personally, I think I’m the extreme of finding it very, very off-putting. But I know it helps and works for A LOT of people.)
I added this question (and the other question you suggested) to the survey I believe you just did. (I figure it was your response since your suggestion about the ED voice was the same as what you wrote above.)
Thanks for sharing these survey results, you definitely received some very eye-opening and heartfelt responses. As an eating disorder treatment provider, we’re always looking for ways to improve our outreach, education, and understanding of our what is really needed by those facing the tough road ahead towards recovery.
Thank you! I’m glad to hear it is helpful and informative. Were there any specific responses (or themes/points) that were eye-opening or unexpected for you? I’m just curious :).